Cracking the Code: Best Practices for Seamless Patient Encounter Tracking

November 30, 2023
Patient Encounter Tracking is a vital piece of medical education. It tracks and catalogs the various procedures, techniques, and experiences a learner has during their time at the institution, so that any issues or gaps in their understanding can be discovered and mitigated.
This week on the Holistic Success Show we welcomed Meegan Carlson, Director of People & Culture at Acuity Insights, to discuss the current state of Patient Encounter Tracking, what changes might improve its effectiveness, and why it’s just as important for the program as it is for the student.
Ready to fill your own ‘gaps’ of knowledge? Read on!
Why is Patient Encounter Tracking important in medical education?
Tracking and documenting clinical experiences is crucial for learners, residents, and fellows in medical training. This helps to ensure exposure to diverse diagnoses procedures, and encounters, aligning with training objectives. It’s important to note that monitoring is often a mandatory accreditation requirement for medical programs, aiding in identifying and addressing gaps in learners’ learning experiences.
What are the key differences between live patient tracking vs. simulated patient tracking?
Whether it’s live or simulated, the typical approach to tracking patient encounters doesn’t usually vary widely. The tracking system should ideally remain consistent for both types of experiences. The crucial aspect is ensuring that the program or learner tracking the encounters can easily confirm what type of patient, diagnoses, or encounter has occurred, when it occurred, and whether it was a live patient or a simulation. This distinction is essential for accurate documentation of clinical experiences.
Why is Patient Encounter Tracking important for programs?
More than just a teaching tool, Patient Encounter Tracking gives insight to a medical program about potential issues or gaps in their curriculum. It is crucial to track where learners are exposed to specific medical procedures or encounters, ensuring alignment with program objectives. For instance, in an emergency medicine rotation, it’s important to verify if learners are witnessing the necessary procedures, or if they are actively participating. If gaps exist, simulations can be utilized to address and supplement these experiences.
What are some of the best practices for a live and simulated Patient Encounter Tracking and how should this data be collected?
When evaluating software for procedure and encounter logging, look for systems that go beyond tracking patient types and clinical skills. It’s crucial to consider the clinical setting and the learner’s level of responsibility. For example, breaking down logs by participation level and patient type can provide valuable insights. Ensuring learners meet program objectives, such as encountering specific patients, can involve a mix of live and simulated experiences. The program should also assess whether the learner observed, participated, or independently performed procedures, tailoring competencies for each encounter type and integrating them effectively into the system structure over time.
What are some of the barriers to adopting Patient Encounter Tracking best practices?
Programs should carefully consider the user experience when setting up tracking systems for learner experiences. The challenge lies in finding a balance between comprehensive data collection and a system that is intuitive and not overly complicated. It’s essential to avoid lengthy and complex data entry forms that hinder the learner’s experience. The system should efficiently guide learners to track diagnoses or procedures, indicate progress toward meeting requirements, and specify the level of competency needed. The ultimate goal is to have an organized and user-friendly system that helps learners stay on track, achieve program objectives, and ensures compliance with accreditation requirements.
What is some advice that would help learners and programs to better utilize Patient Encounter Tracking?
- When setting up a logging system for learner experiences, prioritize alignment with program objectives and competencies. The system should clearly reflect the expected encounters and settings, making it easier for learners to fulfill objectives.
- Consider feedback incorporation, ensuring faculty and senior residents can provide feedback, and determine how it’s collected and shared with trainees.
- Focus on the learner’s experience, opting for a user-friendly tool to capture information without unnecessary complexity, as the impact lies in the people using the system, not just the software itself.
Check out the full episode on Patient Encounter Tracking!
Related Articles

How interviews could be misleading your admissions...
Most schools consider the interview an important portion of their admissions process, hence a considerable…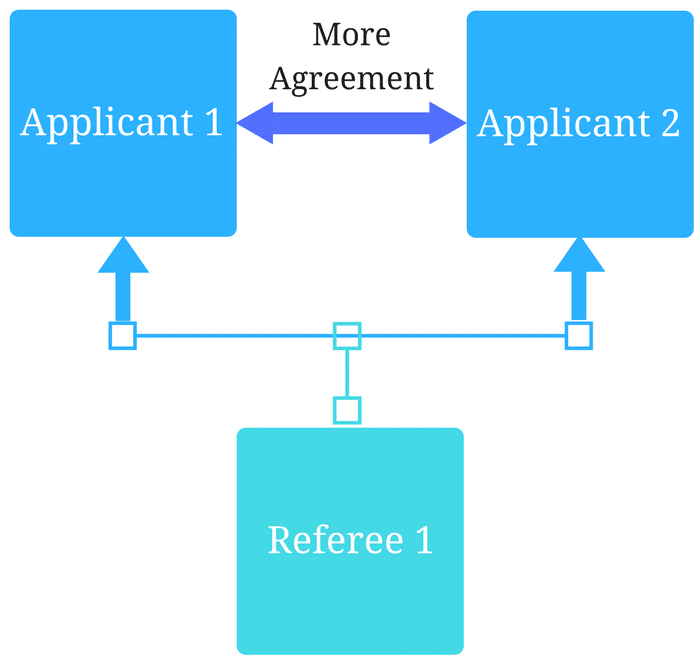
Reference letters in academic admissions: useful o...
Because of the lack of innovation, there are often few opportunities to examine current legacy…
