Exposing the gaps in the residency matching process
August 24, 2021
Match Day is a momentous occasion for medical students; it’s the day they find out where they’ll begin their career in medicine. For final-year trainees in undergraduate medicine though, the months leading up to that day can be exceedingly stressful as they balance clinical rotations with their residency applications, interviews, and audition rotations. Adding to that stress is the fact that the percentage of applicants getting matched with their top-ranked program has dropped seven percent between 2010 and 2020.
The COVID-19 pandemic has only exacerbated these stresses. 2020 saw a notable decline in match outcomes, and while overall match outcomes did improve in 2021, match rates for MD and DO seniors, and IMG applicants all decreased.
Even for those who do match with one of their top choices, a seamless transition to residency is not guaranteed. High rates of burnout are reported among physicians in training, and one systematic review revealed resident well-being is lower than population well-being norms, with demanding schedules, work environment, autonomy, opportunity to build competency, and social relatedness being the greatest factors affecting their well-being.
Given the stresses of Match Day and the overall transition to residency, we’re exploring some of the gaps that exist in the matching system and the ways in which they can be addressed.
Main problems and gaps with residency matching:
1. Application Fever
Over the last 10 years, the number of programs applicants have applied to has nearly doubled. What’s driving it? Researchers believe it can be explained by “behavioral psychology and game theory.” They go on to explain that even with the number of applicants and residency positions being perfectly aligned, “not all positions are equally attractive,” and so applicants will overapply to gain an advantage over others who may be similarly qualified on paper. The problem is that the majority of applicants will use this approach, which does not increase their match outcomes. This strategy is also extremely costly to applicants and can contribute to existing issues in GME selection. On top of that, the sheer number of applications programs receive makes it difficult to assess candidates in a fair and reliable way.
2. Lack of reliable metrics for social intelligence and professionalism
Like many other higher education programs, GME selection teams lack reliable, standardized tools to support holistic applicant review. Things like personal statements and reference letters are cumbersome to review and do not predict their behavior and future professional success. Instead, these programs may rely heavily on the United States Medical Licensure Examination (USMLE) Step 1 and 2 scores to filter and screen large numbers of applicants. The scores were never intended to be used this way, and now USMLE Step 1 is moving to a simple pass/fail, while Step 2 Clinical Skills is being discontinued altogether.
3. Flawed approach to assessing “fit” and preference
Currently, applicants cite desired geographic location, perceived goodness of fit, and program reputation as the top factors for their rankings, but these don’t necessarily contribute to resident success given the high rates of burnout and overall well-being challenges they experience right in their first year, as highlighted above. A learning environment that allows residents to build their autonomy and competence as well as to meaningfully connect with faculty and colleagues is key, but is not reflected in those top three factors.
There is also a lot of uncertainty when it comes to the preference strategy, which can lead to disingenuous rankings and responses for the sake of getting in somewhere. For example, when some programs call students to “express their interest,” which indicates that those applicants are highly ranked, “candidates sometimes latch onto these almost-promises and raise the rank of the calling programs.”
How to improve residency matching
Efforts are already underway to improve resident well-being, comprising both individual and organizational interventions, such as wellness committees and programs, evaluating workplace and workflow interventions, and adherence to the ACGME’s guidelines for duty hours.
As for the matching process, options are still being discussed, including:
- a cap to the total number of programs that applicants can apply to
- a true-preference signaling system, which would allow applicants to select only a small number of programs as preferences
- an early acceptance program that allows some matches to occur before the typical March date
While taking these steps may reduce application fever, it still does not help programs reliably assess personal and professional characteristics or true “fit” that takes into account the importance of the learning environment for residents. That’s why Acuity Insights piloted a comprehensive set of standardized assessments that measure social intelligence, professionalism, and value-alignment with GME programs and applicants in the 2020 and 2021 cycles. The pilot was successful, with both programs and applicants providing positive feedback. These assessments fill a significant void by offering a research-backed method to assess these vital qualities reliably and efficiently, while giving applicants an opportunity to stand out in the early stages of file review and selection, before interviews.

When it comes to “fit” and preference, one of the assessments — Duet — is critical to addressing the uncertainties in the match process by focusing on value alignment. So how does Duet work? Programs first invite various stakeholders (e.g., faculty, administrators, and current residents) to complete the assessment, which results in a single Program Profile that ranks the program’s values and priorities within three categories. Applicants then complete the assessment by selecting the characteristics they most prefer in a program. Finally, programs receive automatic scores that show applicants’ alignment with the program across all categories, which can aid in their review.
Instead of focusing on individual applicants or programs, Duet brings the focus back to what applicants want and need in their education and ties it back to what the program has to offer in training the next generation of physicians. Along with other initiatives, Duet and Casper within Acuity Admissions Assessments can help improve the matching process.
Access the complete results of the Acuity for GME pilot and learn more about Duet
Related Articles

How interviews could be misleading your admissions...
Most schools consider the interview an important portion of their admissions process, hence a considerable…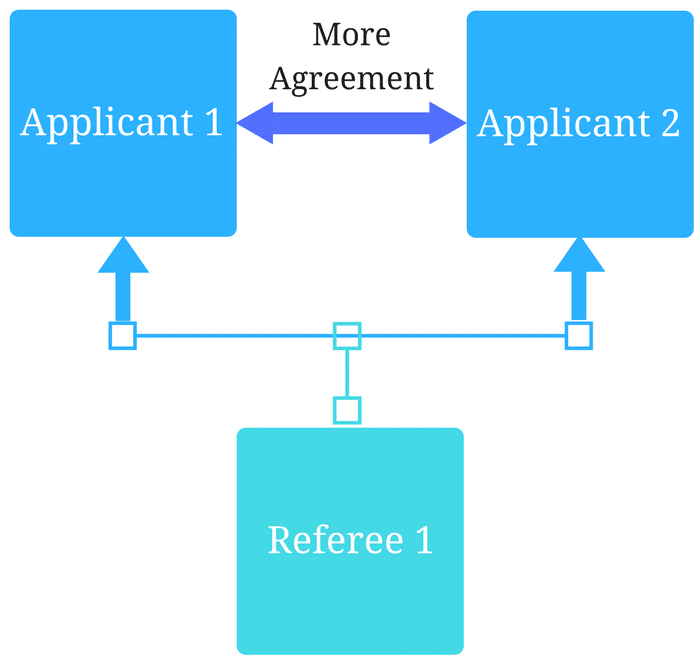
Reference letters in academic admissions: useful o...
Because of the lack of innovation, there are often few opportunities to examine current legacy…
