Standardizing Skills: How EPAs Ensure Residency Readiness
October 18, 2023
The world of medical training is rife with jargon and acronyms, and among them, the term “EPA” stands tall. But what is an EPA, and why should anyone outside of the medical sphere even care?
In yesterday’s Holistic Success Show we dove into all-things EPA – or “entrustable professional activity”, discussing the intricacies of EPAs, debunking common misconceptions, and providing insights into their broader applications across various fields and everyday scenarios.
Sylvia Mioduszewska, Senior Product Manager for One45 at Acuity Insights shared her valuable perspective on the importance of understanding the EPA and applying it correctly with Senior Director, Marketing Anju Visen-Singh.
Read on to discover some of the questions Anju posed to Sylvia.
First of all, what is an EPA?
EPA stands for “entrustable professional activity,” a vital component of competency-based medical education that plays a crucial role in bridging the gap between theoretical knowledge and practical application. EPAs represent tasks that medical trainees, once deemed competent, can carry out independently. Yet, the essence of EPAs stretches beyond the realm of medicine. Whether it’s in a professional setting or in our homes entrusting a teenager with an air fryer, the concept of entrustment is universal.
What are some of the most common misconceptions about EPAs?
Imagine you’re learning to cook. Your ingredient knowledge, recipe interpretation, time management, and every technique you master are like the ‘competencies’ in medical training. These are the foundational skills and knowledge. However, when it comes to making an entire dish, like a delicious lasagna, you need to skillfully combine and integrate all of that knowledge. This is akin to an ‘EPA’ in medical education.
Surprisingly, many mix up foundational skills or competencies with EPAs, but understanding the difference is crucial. Just because you know each ingredient doesn’t mean you can whip up a perfect lasagna on the first try. Similarly, in the medical world, merely having the skills doesn’t mean you can flawlessly perform a comprehensive task like diagnosing a patient. There’s a noted gap in observing and documenting these tasks efficiently, which sometimes causes confusion. Recognizing this distinction is not just about terminology; it’s about making training more effective and ensuring medical professionals are truly ready for the tasks ahead.
How can someone start to figure out whether their EPA is actually an EPA?
Defining an EPA in medical training isn’t as straightforward as it sounds. Essentially, an EPA should be something that can be directly observed and measured in a clinical setting, rather than inferred through an associated competency. For instance, while taking a patient’s history, a trainee should not only showcase their medical knowledge but also integrate competencies like communication skills. The task should be relevant to future practice, and while there are standardized EPAs for undergraduate medical education, requirements can vary significantly between GME specialties, like neurology or pediatrics. If there’s uncertainty about what qualifies as an EPA, it’s always wise to consult educational experts or seasoned clinicians, especially outside the US and Canada where guidelines might not be as clear-cut.
What changes can improve how EPAs are measured in someone’s curriculum or program?
Using technology effectively for real-time EPA assessment is a challenge. While platforms like One45 offer digital solutions, many schools resort to alternatives like survey software. However, it’s essential to use technology tailored for this purpose. While EPAs are intended for immediate assessment, due to various obstacles like tight schedules between patients or lack of connectivity in hospitals, many assessments are postponed until the end of the day. When implementing EPAs, consider the context. Canada’s GME, for instance, uses contextual questions to account for different clinical settings or patient complexities. The design and content of EPAs should be regularly reviewed to ensure they remain aligned with actual clinical practices.
What are the biggest hurdles when transitioning to using EPAs?
Embracing EPAs in medical education can lead to challenges like cultural resistance and a lack of resources. Many institutions, especially where EPAs aren’t mandatory, find it difficult to get faculty buy-in. Faculty often question the validity, requiring additional efforts for training and workshops. These educators, primarily clinician teachers, aren’t necessarily involved in curriculum design, so making EPAs accessible and straightforward for them is crucial. Too many assessments can be overwhelming, but technological advances like voice-to-text feedback can simplify the process.
Implementing EPAs also necessitates robust program management and analytics systems to handle the influx of data they produce. Additionally, a clear understanding of EPAs and how to implement them is vital, given the common confusion between competencies and EPAs. Seeking help from educational consultants or specialized program managers can guide institutions. These challenges might be significant, but the benefits of a well-implemented EPA system are undeniably worth the effort in terms of the UME to GME handoff, as well as into independent practice.
What’s the difference between EPAs for undergraduate medicine (UME) and graduate medicine (GME)?
In medical education, the approach to EPAs varies between UME and GME. In the UME context, EPAs hold significant value. By the end of training, when students are transitioning to residency, program directors should confidently know that these students can perform the essential tasks from day one. This standardization ensures that incoming residents are prepared, allowing residency programs to efficiently begin without re-verifying foundational skills.
What are three critical factors for effective EPAs for any program?
In reflecting on the intricacies of Entrustable Professional Activities (EPAs) and their successful implementation in medical education, three pivotal factors emerge. Firstly, faculty development is non-negotiable. Without the full backing and understanding of your faculty, your EPAs remain theoretical. Their support is the bedrock of success. Additionally, the right technology is vital. A system that collects and reports data efficiently can alleviate countless potential challenges, ensuring smooth progress. Lastly, the chosen entrustment scale is crucial. It’s imperative to select one that aligns with the specific requirements and expectations of the educational level, be it UME or GME. Entrustment is incremental, and finding a scale that faculty are comfortable with can make all the difference. In essence, the seamless integration of EPAs hinges on these cornerstones: engaged faculty, robust technology, and a suitable entrustment scale. With these in place, the path to fostering competent medical professionals becomes clearer.
To listen to the full episode on the value of EPAs, visit our YouTube channel.
Related Articles

How interviews could be misleading your admissions...
Most schools consider the interview an important portion of their admissions process, hence a considerable…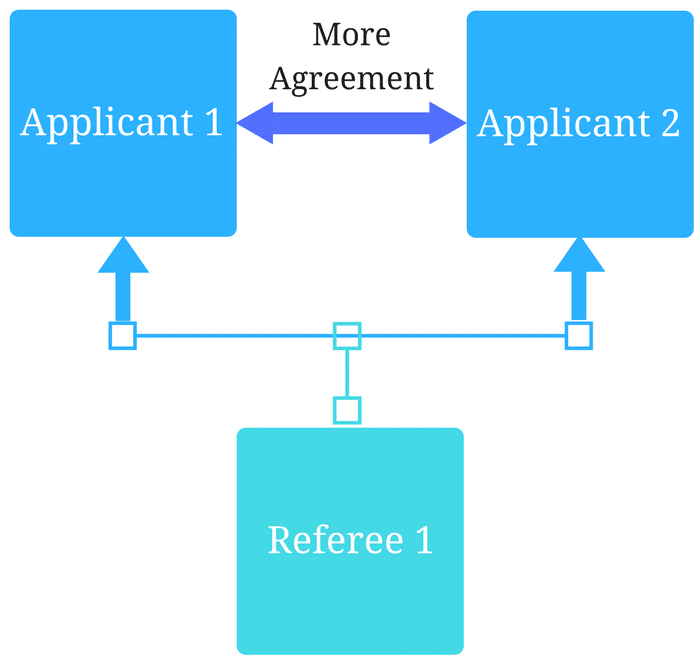
Reference letters in academic admissions: useful o...
Because of the lack of innovation, there are often few opportunities to examine current legacy…
